Skin and Wound Care
Select a Skill:
- » Applying Elastic Stockings
- » Giving a Back Massage
- » Assisting with Pressure Ulcer Prevention and Care
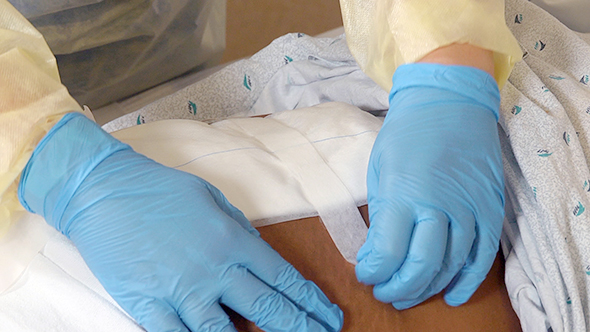
- » Applying a Dry, Non-sterile Dressing
Take the Review Test:

Purpose
- Wound dressings have many functions. They:
- Protect wounds from injury and microbes.
- Absorb drainage.
- Remove dead tissue.
- Promote comfort.
- Cover unsightly wounds.
- Provide a moist environment for wound healing.
- Apply pressure (pressure dressings) to control bleeding.
- Dressings are described by the material used and how they are applied. Common dressing products are gauze, non-adherent gauze, and transparent adhesive film. Dressings are dry or wet.
- Some agencies let you apply simple, dry, non-sterile dressings to simple wounds. Follow these rules:
- Let pain-relief drugs take effect, usually 30 minutes. The dressing change can cause discomfort. The nurse gives the drugs and tells you how long to wait.
- Meet fluid and elimination needs before you begin.
- Collect equipment and supplies before you begin.
- Do not bend or reach over your work area.
- Control your verbal and nonverbal reactions to any unpleasant wound odor, appearance, or drainage.
- Remove soiled dressings so the person cannot see the soiled side. The drainage and its color may upset the person.
- Do not force the person to look at the wound. A wound can affect body image and self-esteem. The nurse helps the person deal with the wound.
- Remove tape by pulling it toward the wound.
- Remove dressings gently. If the dressing sticks, the nurse may have you wet the dressing with saline solution. A wet dressing is easier to remove.
- Touch only the outer edges of old and new dressings.
Equipment
Roll cursor over items to see labels. For the purposes of clearly depicting the equipment, a barrier is not shown in this photo. When providing care, a barrier should always be placed on the surface before placing the equipment.

Tape
Bath blanket
Gloves
Gown
Adhesive remover
Saline solution as directed by the nurse
4x4 gauze squares
Dressing set with scissors and forceps
Montgomery ties
Delegation
- Follow delegation guidelines. Before applying a dry, non-sterile dressing, obtain this information from the nurse and care plan:
- When to change the dressing
- When the person received a pain-relief drug and when it will take effect
- What to do if the dressing sticks to the wound
- How to clean the wound
- What dressings to use
- How to secure the dressing—tape or Montgomery ties
- What kind of tape to use—adhesive, paper, plastic, cloth, or elastic
- What size tape to use—½, ¾, 1, 2, or 3 inch width
- What observations to report and record
- When to report observations
- What patient or resident concerns to report at once
Preparation

- Observe quality-of-life measures.
- Review the information under Delegation and Safety and Comfort.
- Practice hand hygiene.
- Collect the equipment.
- Practice hand hygiene.
- Identify the person. Check the ID bracelet against the assignment sheet. Also call the person by name.
- Provide for privacy.
- Arrange your work area. You should not have to reach over or turn your back on your work area.
- Raise the bed for body mechanics. Bed rails are up if used.
Safety

- Contact with blood, body fluids, secretions, or excretions is likely. Follow Standard Precautions and the Bloodborne Pathogen Standard. Wear PPE as needed.
- Do not apply tape to irritated, injured, or non-intact skin. Tape can further damage the skin.
Comfort
- Wounds and dressing changes can cause discomfort or pain. The nurse may give a pain-relief drug before the dressing change. Allow time for the drug to take effect. Gently apply and remove tape and dressings.
- The person may not report discomfort from a dressing. You should ask:
- “Is the dressing comfortable?”
- “Does the tape cause pain or itching?”
Procedure Video
Audio Description: OFFFollow-up Care

- Provide for comfort.
- Place the call light within reach.
- Lower the bed to a safe and comfortable position for the person. Follow the care plan.
- Raise or lower bed rails. Follow the care plan.
- Return equipment and supplies to their proper place. Leave extra dressings and tape in the room.
- Discard used supplies into the bag. Tie the bag closed. Discard the bag following agency policy. (Wear gloves for this step.)
- Clean your work area. Follow the Bloodborne Pathogen Standard.
- Unscreen the person.
- Complete a safety check of the room.
- Remove and discard gloves. Practice hand hygiene.
Reporting/Recording
- Report and record your observations, including:
- What you used to dress the wound and secure the dressing
- A red or swollen wound or a warm area around it
- If wound edges are closed or separated or if a wound has broken open
- Drainage amount and appearance—clear, bloody, or watery and blood-tinged; thick and green, yellow, or brown
- Wound or drainage odor
- Intactness and color of surrounding tissues
- Possible dressing contamination, such as with urine or feces
- Pain or fever
Review Questions
Select the best answer.
1. What is the purpose of applying a dry, non-sterile dressing?
 To prevent contact with blood or body fluids
To prevent contact with blood or body fluids To cover a wound and protect it from injury and microbes
To cover a wound and protect it from injury and microbes To prevent skin breakdown over a body area, such as the ankle or hip
To prevent skin breakdown over a body area, such as the ankle or hip To cover medicated creams or ointments and prevent the spread of infection
To cover medicated creams or ointments and prevent the spread of infection
Select the best answer.
2. After applying a dry, non-sterile dressing, which observation should you report to the nurse?
Select the best answer.
3. Which action is appropriate when changing a dry, non-sterile dressing?
 Encourage the person to participate in care by having him or her apply the clean dressing and tape.
Encourage the person to participate in care by having him or her apply the clean dressing and tape. Remove the tape from the dressing by holding the skin down and pulling the tape quickly away from the wound.
Remove the tape from the dressing by holding the skin down and pulling the tape quickly away from the wound. Remove the old dressing all at once, holding the soiled side so the person can see the amount of drainage present.
Remove the old dressing all at once, holding the soiled side so the person can see the amount of drainage present. Help the person into a comfortable position, cover him or her with a bath blanket, and expose only the affected body part.
Help the person into a comfortable position, cover him or her with a bath blanket, and expose only the affected body part.
Select the best answer.
4. If the nurse gives the person a pain-relief drug, how long should you expect to wait before changing the person’s dressing?
Select the best answer.
5. When removing a dry, non-sterile dressing, you notice that it is sticking to the person’s wound. What should you do?
 Moisten the dressing with saline solution.
Moisten the dressing with saline solution. Pull off the dressing quickly to minimize pain.
Pull off the dressing quickly to minimize pain. Apply adhesive remover on a 4 x 4 gauze square.
Apply adhesive remover on a 4 x 4 gauze square. Postpone the dressing change until the wound heals.
Postpone the dressing change until the wound heals.
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

