Skin and Wound Care
Select a Skill:
- » Applying Elastic Stockings
- » Giving a Back Massage
- » Assisting with Pressure Ulcer Prevention and Care
- » Applying a Dry, Non-sterile Dressing
Take the Review Test:

Purpose

- A pressure ulcer is a lesion caused by unrelieved pressure that damages underlying tissues. It also may be called a decubitus ulcer, bed sore, or pressure sore.
- Pressure is the major cause of pressure ulcers. For example, unrelieved pressure on the skin between a bony area and a hard surface can prevent blood flow to that area. Oxygen and nutrients cannot get to the cells. Skin and tissues die.
- Shearing and friction contribute to pressure ulcers by causing skin breakdown. Shearing occurs when the person slides down in the bed or chair. Friction scrapes the skin, causing an open area that needs to heal.
- Risk factors include breaks in the skin, poor circulation to an area, moisture, dry skin, and irritation by urine and feces. Persons at risk for pressure ulcers are those who:
- Are bedfast (confined to a bed) or chairfast (confined to a chair).
- Need some or total help in moving.
- Are agitated or have involuntary muscle movements.
- Have urinary or fecal incontinence.
- Are exposed to moisture.
- Have poor nutrition.
- Have poor fluid balance.
- Have lowered mental awareness.
- Have problems sensing pain or pressure.
- Have circulatory problems.
- Are obese or very thin.
- Have a healed pressure ulcer.
- Bony prominences (pressure points) are particularly susceptible to pressure ulcers.
- Preventing pressure ulcers is easier than trying to heal them. Prevention involves:
- Identifying persons at risk.
- Implementing prevention measure for those at risk.
- To treat pressure ulcers, the doctor orders wound care products, drugs, treatments, and special equipment to promote healing.
Equipment
Roll cursor over items to see labels. For the purposes of clearly depicting the equipment, a barrier is not shown in this photo. When providing care, a barrier should always be placed on the surface before placing the equipment.

Dirty linen hamper
Towels
Wedge cushion
Pillow
Basin
Body wash
Lotion
Washcloths
Gloves
Powder
Elbow protectors
Incontinence products
Barrier cream
Delegation
- Follow delegation guidelines. Before assisting with pressure ulcer prevention and care, ensure that:
- The state law allows a nursing assistant to perform this procedure.
- The procedure is in your job description.
- You have been taught how to perform the procedure.
- A nurse is available for supervision and questions.
- Before assisting with pressure ulcer prevention and care, obtain this information from the nurse and care plan:
- Which wound care products to use
- What treatments you may provide or assist with
- What special equipment or protective devices the person needs
- What dressing to use
- Which tool to use for assessing pressure ulcers or the risk of pressure ulcers
- What measures to take to prevent skin breakdown and pressure ulcers
- What observations to report and record
- When to report observations
- What patient or resident concerns to report at once
Preparation

- Observe quality-of-life measures.
- Review the information under Delegation and Safety and Comfort.
- Practice hand hygiene.
- Identify the person. Check the ID bracelet against the assignment sheet. Also call the person by name.
- Collect the equipment.
- Provide for privacy.
- Raise the bed for body mechanics. Bed rails are up if used.
Safety

- If open skin or drainage is present, do not perform any treatment. Notify the nurse.
- Follow Standard Precautions and the Bloodborne Pathogen Standard if the person has an open area on the skin.
Comfort
- Pressure ulcers can cause pain. Pain management is important. Pain may affect movement and activity. Immobility is a risk factor for pressure ulcers. And it may delay healing of an existing pressure ulcer.
- Be gentle with the person’s skin when lifting or moving.
Procedure Video
Audio Description: OFFFollow-up Care
- Provide for comfort.
- Place the call light within reach.
- Lower the bed to its lowest position. Raise or lower bed rails. Follow the care plan.
- Return any supplies and equipment to their proper places.
- Unscreen the person.
- Complete a safety check of the room.
- Follow agency policy for dirty linens.
- Remove your gloves (if worn) and practice hand hygiene.
Reporting/Recording
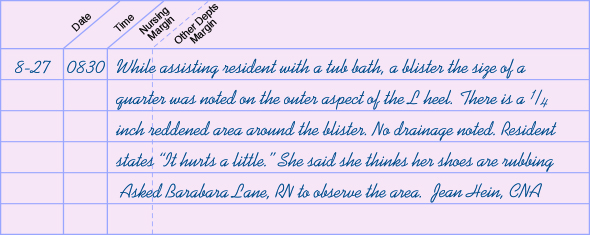
- Report and record your observations. If you see areas of redness, skin color changes, blisters, or skin or tissue loss, describe them fully, including the:
- Location, such as “on the left heel”
- Skin condition, such as “intact, but red and warm”
- Size compared to a familiar object, such as “the size of a quarter”
- Amount and color of any drainage
- Odor, if present
- Soiled or missing dressings
Review Questions
Select the best answer.
1. Which action is appropriate when assisting with pressure ulcer care?
 Wash the area with disinfecting soap and vigorously dry it
Wash the area with disinfecting soap and vigorously dry it Using cool lotion, firmly massage the skin over the reddened area
Using cool lotion, firmly massage the skin over the reddened area Stop the procedure and notify the nurse if the person has open areas
Stop the procedure and notify the nurse if the person has open areas Apply an antibacterial cream to the area and cover with a sterile dressing
Apply an antibacterial cream to the area and cover with a sterile dressing
Select the best answer.
2. Which person has the lowest risk of developing a pressure ulcer?
 A woman with oliguria
A woman with oliguria A woman with malnutrition
A woman with malnutrition A man with fecal incontinence
A man with fecal incontinence A man with a healed pressure ulcer
A man with a healed pressure ulcer
Select the best answer.
3. What is the major cause of pressure ulcers?
Select the best answer.
4. What is another name for a pressure ulcer?
Select the best answer.
5. Which protective device may be used to prevent and treat pressure ulcers?
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

