Measurements and Vital Signs
Select a Skill:
- » Measuring Weight and Height
- » Taking a Radial Pulse
- » Taking an Apical Pulse
- » Counting Respirations
- » Taking a Temperature with an Electronic Thermometer
- » Measuring Blood Pressure
- » Using a Pulse Oximeter
Take the Review Test:
Purpose
- Pulse oximetry measures the oxygen (O2) concentration in arterial blood. Oxygen concentration is the amount (percent) of hemoglobin containing O2. The normal range is 95% to 100%. For example, if 97% of all hemoglobin (100%) carries O2, tissues get enough oxygen. If only 90% contains O2, tissues do not get enough.
- A sensor attaches to a finger, toe, earlobe, nose, or forehead. A good sensor site is needed. Avoid swollen sites and sites with skin breaks. Sometimes blood flow to the fingers or toes is poor. Then the earlobe, nose, and forehead sites are used.
- Nail polish, fake nails, and movements affect measurements. Remove nail polish or use another site. Do not use a finger site if the person has fake nails. Blood pressure cuffs affect blood flow. If using a finger site, do not measure blood pressure on that side.
- Oxygen concentration is often measured with vital signs. Or it is monitored continuously. Alarms are set for continuous monitoring. An alarm sounds if the O2 concentration is low. Report and record oxygen concentration according to agency policy. An agency may use one of these terms:
- Pulse oximetry or pulse ox
- O2 saturation or O2 sat
- SpO2 (saturation of peripheral oxygen)
Equipment
Roll cursor over items to see labels. For the purposes of clearly depicting the equipment, a barrier is not shown in this photo. When providing care, a barrier should always be placed on the surface before placing the equipment.

Oximeter and sensor
Tape
Towel
Delegation
- Follow delegation guidelines. Before using a pulse oximeter, obtain this information from the nurse and care plan:
- What site to use
- How to use the equipment
- What sensor to use
- What type of tape to use, if needed
- The person’s normal range of SpO2
- Alarm limits for SpO2 and pulse rate, if set
- When to do the measurement
- How often to check the sensor site—usually every 2 hours
- What observations to report and record
- When to report observations
- What patient or resident concerns to report at once
Preparation

- Observe quality-of-life measures.
- Review the information under Delegation and Safety and Comfort.
- Practice hand hygiene.
- Collect the equipment.
- Arrange your work area.
- Identify the person. Check the ID bracelet against the assignment sheet. Also call the person by name.
- Provide for privacy.
Safety

- The person’s condition can change quickly. Pulse oximetry does not lessen the need for good observations. Observe for signs and symptoms of hypoxia and altered respiratory system function, such as abnormal breathing patterns. These patterns may include:
- Tachypnea (rapid breathing)
- Bradypnea (slow breathing)
- Apnea (no breathing)
- Cheyne-Stokes respirations (respirations that increase in rate and depth and then become shallow and slow)
- Kussmaul respirations (deep, rapid respirations)
Comfort
- A clip-on sensor feels like a clothespin. It should not hurt or cause discomfort. Ask the person to tell you at once if it causes pain, discomfort, or too much pressure. Change the sensor site as directed by the nurse.
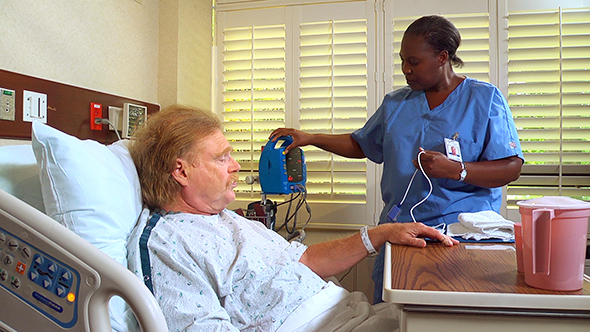
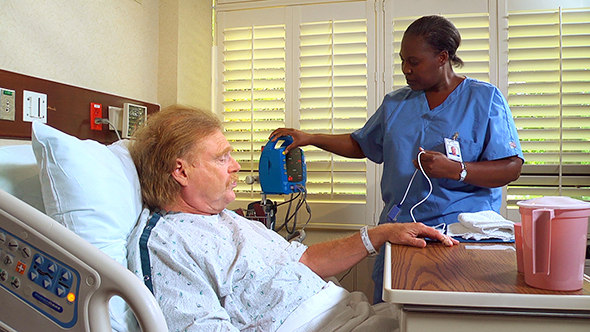
Procedure Video
Audio Description: OFFFollow-up Care

- Provide for comfort.
- Place the call light within reach.
- Unscreen the person.
- Complete a safety check of the room.
- Return the device to its proper place (unless monitoring is continuous).
- Practice hand hygiene.
Reporting/Recording
- Report and record your observations, including:
- The date and time
- The SpO2 and display pulse rate
- Apical or radial pulse rate
- What the person was doing at the time
- Oxygen flow rate and the device used
- Reason for the measurement: routine, continuous monitoring, or condition change
- Report patient or resident concerns at once:
- An SpO2 below the alarm limit (usually 95%)
- A pulse rate above or below the alarm limit
- Presence of signs and symptoms of hypoxia, such as dizziness, agitation, increased pulse and respiratory rates, forward-leaning position, cyanosis (bluish skin, lips, mucous membranes, and nail beds), and dyspnea
Review Questions
Select the best answer.
1. What does pulse oximetry measure?
 The rate and force of the person’s pulse
The rate and force of the person’s pulse The amount of oxygen in the person’s lungs
The amount of oxygen in the person’s lungs The amount of oxygen in the person’s blood
The amount of oxygen in the person’s blood The amount of carbon dioxide in the person’s blood
The amount of carbon dioxide in the person’s blood
Select the best answer.
2. On the digital readout of a pulse oximeter, what is the normal oxygen concentration?
Select the best answer.
3. Which factor may interfere with the pulse oximetry reading?
Select the best answer.
4. When using a pulse oximeter, which measurements should you compare?
 The person’s radial pulse rate and the oximeter’s pulse rate
The person’s radial pulse rate and the oximeter’s pulse rate The person’s blood pressure and the oximeter’s blood pressure
The person’s blood pressure and the oximeter’s blood pressure The person’s respiratory rate and the oximeter’s respiratory readout
The person’s respiratory rate and the oximeter’s respiratory readout The person’s temperature and the oximeter’s temperature waveform
The person’s temperature and the oximeter’s temperature waveform
Select the best answer.
5. During pulse oximetry, which finding should you report at once?
You have completed the Review Questions for this skill. To take the Review again select the Start Over button. To proceed to another skill select from the dropdown menu. Select the Home or Back button to proceed to the next section.

